Advances in radiotherapy technology are making cancer treatment more powerful, more precise and easier to deliver. While this means new benefits for patients, it also opens the door to new safety challenges.
“Introducing new technology doesn’t come without its risks. The issue with each new machine is the possibility of making errors because radiotherapy professionals are still learning how the machine really works. They can’t simply trust that it will do what it should do. They need to verify it, ideally through elaborate testing,” said Christoph Trauernicht, Head of the Medical Physics Division at Tygerberg Hospital and Senior Lecturer at Stellenbosch University in Cape Town.
Since the early 20th century, radiation has played a growing and increasingly indispensable role in cancer treatment. Radiation therapy, or radiotherapy, involves targeting very precise doses of radiation at tumours to kill cancer cells. This can be done with external beams of radiation, such as X-rays, gamma rays or electrons, or by using radioactive sources placed inside or on a patient.
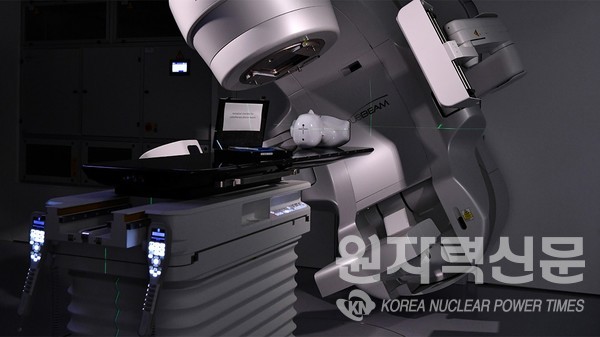
Today, the most commonly used machine to treat cancer with radiation is the linear accelerator, or linac for short. There are more than 12 000 linacs in operation in hospitals worldwide, and their prevalence is only expected to increase.
“As technology continues to advance, it becomes even more important that radiotherapy is provided safely. New technology allows for more automation and complex optimization of radiation doses but also requires additional professional training and different safety systems to ensure that patients are treated correctly,” said Debbie Gilley, Radiation Protection Specialist at the IAEA.
About 50% of cancer patients receive radiation therapy at some point during their treatment. As the number of new cancer cases continues to rise, so will the need for radiotherapy. This also means medical physicists and resources for their training in radiation protection will continue to play a growing role in ensuring the safe and effective use of radiation in medicine.
The IAEA supports countries worldwide in adapting to evolving technologies and safety needs. It has several initiatives in place to strengthen the field of medical physics through the publication of guidelines and factsheets, organization of seminars for health professionals and decision makers, and collaboration with professional societies.
This work is guided by the IAEA’s overall efforts to improve access to quality radiotherapy, which includes assisting countries in applying IAEA safety standards on radiation safety. These standards have been developed in close cooperation with governments and organizations around the world and are periodically revised and updated by experts to account for technological advances and new knowledge.
The IAEA has supported the training of radiation health professionals in Africa so that they can safely and effectively embrace new machines in order to expand imaging and radiotherapy services and to shrink gaps in access to care.
“South Africa is a varied landscape when it comes to patients’ access to radiotherapy services. There’s a large disparity between the public and private sector, with some public sector patients having to wait several months to receive treatment. That’s something we’re working on changing,” said Trauernicht.
Tygerberg Hospital, one of the biggest specialist hospitals in South Africa, treats roughly 1600 patients with radiotherapy every year. The hospital acquired its fourth linac in 2019. Every linac that arrives at the facility must, in line with safety regulations, go through a process of acceptance testing, commissioning and licensing before it is used on patients. This includes the installation of the machine in a specially designed room, commissioning of the treatment planning system and the training of staff.
“By acquiring new radiotherapy machines, among other changes to our services, we’re hoping to shorten waiting times, possibly shorten treatment times and therefore allow for a quicker throughput of patients. Of course, adequate staffing is also needed,” Trauernicht said.
But advancing radiotherapy itself is not the only aspect of radiation safety, added Trauernicht. “A strong national regulatory body is key to safety implementation at the institutional level. In South Africa, we have national societies for medical physics, radiography, oncology, radiology and nuclear medicine physicians, which all play a very important role in ensuring safety. They are trying to further build awareness related to regulations around the country.”
South Africa continues to refine its regulatory framework to ensure close adherence to the IAEA’s safety standards. Current regulations stipulate that medical physicists must be involved in radiotherapy and that safety programmes should be developed and implemented. In parallel, regional activities are gaining momentum through efforts such as the AFROSAFE campaign to increase radiation protection education and the efforts of the Federation of African Medical Physics Organisations towards the accreditation of medical physics training programmes.

